NR 661 Week 4 Vise Assignment Study Guide
-
$15.00
| Institution | NR 661 APN Capstone Practicum |
| Contributor | Shanzay |
Preview.........1st Page
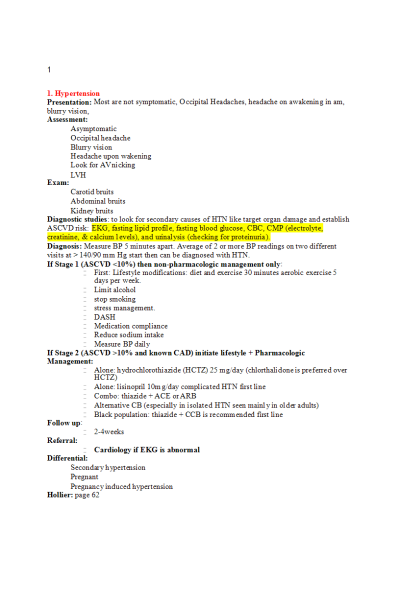
- Hypertension
Presentation: Most are not symptomatic, Occipital Headaches, headache on awakening in am, blurry vision,
Assessment:
- Asymptomatic
- Occipital headache
- Blurry vision
- Headache upon wakening
- Look for AV nicking
- LVH
Exam:
- Carotid bruits
- Abdominal bruits
- Kidney bruits
Diagnostic studies: to look for secondary causes of HTN like target organ damage and establish
ASCVD risk: EKG, fasting lipid profile, fasting blood glucose, CBC, CMP (electrolyte, creatinine, & calcium levels), and urinalysis (checking for proteinuria).
Diagnosis: Measure BP 5 minutes apart. Average of 2 or more BP readings on two different visits at > 140/90 mm Hg start then can be diagnosed with HTN.
If Stage 1 (ASCVD <10%) then non-pharmacologic management only:
- First: Lifestyle modifications: diet and exercise 30 minutes aerobic exercise 5 days per week.
- Limit alcohol
- stop smoking
- stress management.
- DASH
- Medication compliance
- Reduce sodium intake
- Measure BP daily
If Stage 2 (ASCVD >10% and known CAD) initiate lifestyle + Pharmacologic
Management:
- Alone: hydrochlorothiazide (HCTZ) 25 mg/day (chlorthalidone is preferred over HCTZ)
- Alone: lisinopril 10mg/day complicated HTN first line
- Combo: thiazide + ACE or ARB
- Alternative CB (especially in isolated HTN seen mainly in older adults)
- Black population: thiazide + CCB is recommended first line
Follow up:
- 2-4weeks
Referral:
- Cardiology if EKG is abnormal
Differential:
- Secondary hypertension
- Pregnant
- Pregnancy induced hypertension
Hollier: page 62
- Hyperlipidemia
Etiology: may be familial, dietary, obesity, hypothyroid, renal disorders, thiazide or beta blocker use, alcohol and/or caffeine intake
Presentation: few physical findings
- Xanthomata (lipid deposits around the eyes)
- Corneal Arcus prior to age 50 years (white iris), normal
- Angina
- Bruits
- MI
- Stroke
Diagnostics:
- Fasting/nonfasting lipid profile (total cholesterol, LDL, and HDL minimally affected by eating)
- Glucose,
- UA and creatinine (for detection of nephrotic syndrome which can induce dyslipidemia),
- TSH (for detection of hypothyroidism)
Diagnosis: Pt with LDL >= 190mg/dL
Non-pharmacologic Management:
- Lifestyle Modification; diet and exercise.
Pharmacologic Management
Those who benefit most from statin therapy include:
- hx of CVD or stroke,
- LDL 190 or greater,
- DM with LDL 70-189,
- no evidence of ASCVD or DM but have LDL 70-189 PLUS an estimated ASCVD risk of 7% or greater
- High risk:
- Atorvastatin 40 or 80 mg daily
- Rosuvastatin 20 or 40 mg daily
- Moderate risk:
- Atorvastatin 10 or 20 mg daily
- (other statin medications also listed in Hollier)
- If statins not tolerated, temporarily stop, decrease dose, and re-challenge with 2-3 statins of differing metabolic pathways and intensities.
Follow up:
- after initiating therapy, follow-up every 6-8 weeks until goal attained then every 6-12 months to evaluate compliance
- evaluate lipids every 5 years starting at age 20 if normal values obtained
Refer: Nutritionist
Differentials: consider secondary causes
- Hypothyroidism
- Pregnancy
- Diabetes
- Non-fasting state
Hollier: page 55
| Instituition / Term | |
| Term | Year 2022 |
| Institution | NR 661 APN Capstone Practicum |
| Contributor | Shanzay |